- Industry Solutions
Industry Solutions
From reshaping the quote to cash process, to transforming engagement with channels partners, to achieving excellence in global product launch, Model N enables digital reinvention with industry-specific solutions that maximize revenue.
- Right block
- Industry Solutions
Industry Solutions
From reshaping the quote to cash process, to transforming engagement with channels partners, to achieving excellence in global product launch, Model N enables digital reinvention with industry-specific solutions that maximize revenue.
- Right block
- Products
Our Products
Model N delivers a platform for business reinvention, empowering companies to maximize revenue as they transform Sales, Marketing, Channels, Finance, and Legal processes.
- Right block
- Services & Support
Services & Support
To ensure you get the most out of your Model N investment Model N provides a complete set of professional Customer Success, Services and Support offerings designed to further your business and IT success.
- Right block
- Resources
- Resources
2025 State of Revenue Report
How do leaders plan to optimize revenue in 2025?
Eighty-seven percent of business leaders state that their company is focusing its innovation plans on automating revenue management operations. Learn how you can create smarter, more efficient revenue processes.
- Right block
- Resources
- Company
Company
Model N supports the complex business needs of the world’s leading brands in pharmaceutical, medical device, high tech, manufacturing and semiconductors across more than 120 countries, including Pfizer, AstraZeneca, Sanofi, Gilead, Abbott, AMD, Micron, Seagate, STMicroelectronics, NXP, Sesotec, and Southern States.
- Right block
Contact Sales












 Whitepaper
Whitepaper

 On-Demand Webinar
On-Demand Webinar
 Solution Brief
Solution Brief


.
- Products
Our Products
Model N delivers a platform for business reinvention, empowering companies to maximize revenue as they transform Sales, Marketing, Channels, Finance, and Legal processes.
- Right block
- Services & Support
Services & Support
To ensure you get the most out of your Model N investment Model N provides a complete set of professional Customer Success, Services and Support offerings designed to further your business and IT success.
- Right block
- Resources
- Resources
2025 State of Revenue Report
How do leaders plan to optimize revenue in 2025?
Eighty-seven percent of business leaders state that their company is focusing its innovation plans on automating revenue management operations. Learn how you can create smarter, more efficient revenue processes.
- Right block
- Resources
- Company
Company
Model N supports the complex business needs of the world’s leading brands in pharmaceutical, medical device, high tech, manufacturing and semiconductors across more than 120 countries, including Pfizer, AstraZeneca, Sanofi, Gilead, Abbott, AMD, Micron, Seagate, STMicroelectronics, NXP, Sesotec, and Southern States.
- Right block
- Industry Solutions
Industry Solutions
From reshaping the quote to cash process, to transforming engagement with channels partners, to achieving excellence in global product launch, Model N enables digital reinvention with industry-specific solutions that maximize revenue.
- Right block
- Products
Our Products
Model N delivers a platform for business reinvention, empowering companies to maximize revenue as they transform Sales, Marketing, Channels, Finance, and Legal processes.
- Right block
- Services & Support
Services & Support
To ensure you get the most out of your Model N investment Model N provides a complete set of professional Customer Success, Services and Support offerings designed to further your business and IT success.
- Right block
- Resources
- Resources
2025 State of Revenue Report
How do leaders plan to optimize revenue in 2025?
Eighty-seven percent of business leaders state that their company is focusing its innovation plans on automating revenue management operations. Learn how you can create smarter, more efficient revenue processes.
- Right block
- Resources
- Company
Company
Model N supports the complex business needs of the world’s leading brands in pharmaceutical, medical device, high tech, manufacturing and semiconductors across more than 120 countries, including Pfizer, AstraZeneca, Sanofi, Gilead, Abbott, AMD, Micron, Seagate, STMicroelectronics, NXP, Sesotec, and Southern States.
- Right block
Quick Links
- Products
- Life Science – Pharma
- Payer Management
Payer Management
Reduce risk with your payer and pharmacy benefit manager contracting processes.
View Solution BriefPharma companies pay an average 25 to 31% of their revenue in rebates with heavy penalties for late payments.
- Accurate, timely rebate and fee validation, calculation, and settlement are crucial to maintaining profitability.
- Rebates are becoming more innovative and value-based, creating operationally complex agreements that are difficult to execute.
- Treatment methodologies are becoming complicated and complex, impacting claims processing.
- As exposure to regulatory programs grows, the risk of overpayments doubles.
- Manual processes and disconnected spreadsheet-based tools hamper efforts to navigate complex requirements for formulary, market share, and price protection calculations.

How Model N Payer Management solution helps you
With Payer Management, you can optimize revenue and ensure compliance with your payer agreements.
Increased visibility
Gain visibility and control into your payer revenue management process to ensure the right payers are getting the right discounts.
Improved margins
Maximize revenue by reducing rebate overpayments and rejecting invalid claims.
Reduced effort
Rely on a single platform for handling all aspects of contracts and pricing management, formulary management, and plan management.
Scalability
Ability to scale to the most demanding needs of the largest manufacturers in the world. From managing PBMs to Plan relationships and executing simple to complex rebate programs.
Trusted by leading pharma innovators




Looking for more information?
Maximize revenue with a comprehensive, cloud-based solution
Model N Payer Management with Validata offers value beyond pricing by supporting flexible contracts, enforcing agreement terms, and delivering robust analytics for payments and reporting.
New price protection calculation results screen
Gain visibility into the entire price protection calculation and the results of the evaluation.
Strategy designer
Leverage key data (prescription, sales, clinical, etc.) to build strategies for creating and implementing pricing, rebates, and accurate calculations.
Templates and clauses
Improve governance and reduce exposure to risk with preapproved contract templates and clauses, approval workflows, and version tracking.
Single repository
Reduce manual effort by keeping all structured contract documents in a single location.
Data visibility
Determine effectiveness and accuracy with a clear line of sight into claims processing.
Streamline and automate your entire revenue management process
Model N Payer Management is the only end-to-end industry-leading payer management solution. It is a core component of Model N Revenue Cloud for Pharma, a suite of the most comprehensive solutions that meet the needs of the pharmaceutical industry.
- End revenue leakage in payer contracting and rebating processes.
- Optimize 100% of your global revenue with detailed visibility across all channels.
- Ensure contract compliance.
- Remain focused on bringing innovative, life-changing products to market.
Add On's
Related products
Looking for more information?
Related resources

2025 State of Revenue Report
The 7th annual State of Revenue Report reveals the power of data and analytics in optimizing life sciences and high-tech revenue. VIEW Whitepaper
Barrier Lifted? CMS Proposed Rule on Value-Based Purchasing Agreements
Learn about the latest proposed CMS rule to move toward paying based on value instead of volume. Watch Now

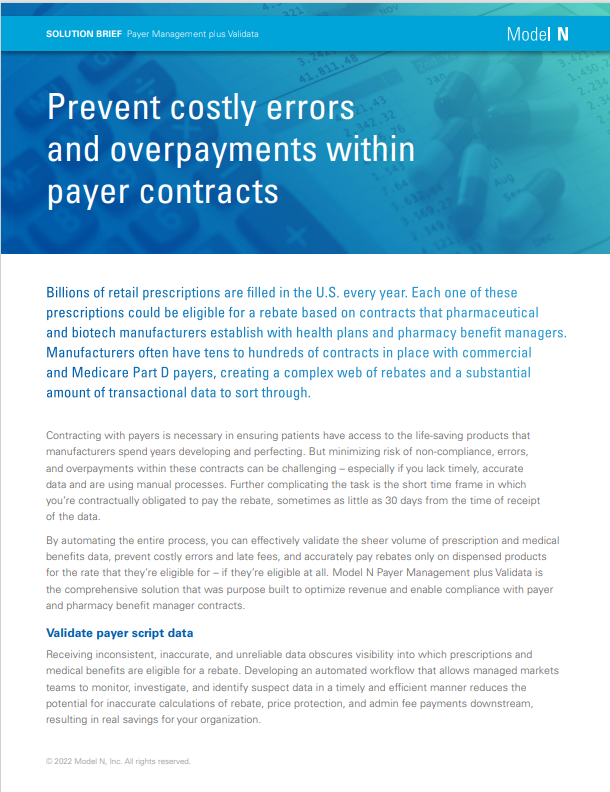
Payer Management Solution Brief
Prevent costly errors and overpayments within payer contracts VIEW Solution Brief
Powering Innovators
Enabling our Customers to Deliver Life-Changing Products to the World
Contact Sales
Thank you for your interest in Model N. Please submit the form and our sales team will contact you within 24 hours.
Our Customers Include:
Thank you for reaching out.
We look forward to responding within one business day.